Neisseria Meningitidis' Key Protein: PorA's Role in Pathogenesis & Vaccine Development
Explore the pivotal role of PorA, a major outer membrane protein of Neisseria meningitidis, in bacterial pathogenesis, immune evasion, and vaccine development. Learn about PorA's structural features, host cell interactions, and therapeutic potential, shaping the future of meningococcal disease management.
Understanding Neisseria meningitidis: A Crucial Insight into Bacterial Membranes and Porins
Introduction: Neisseria meningitidis and its Impact on Human Health

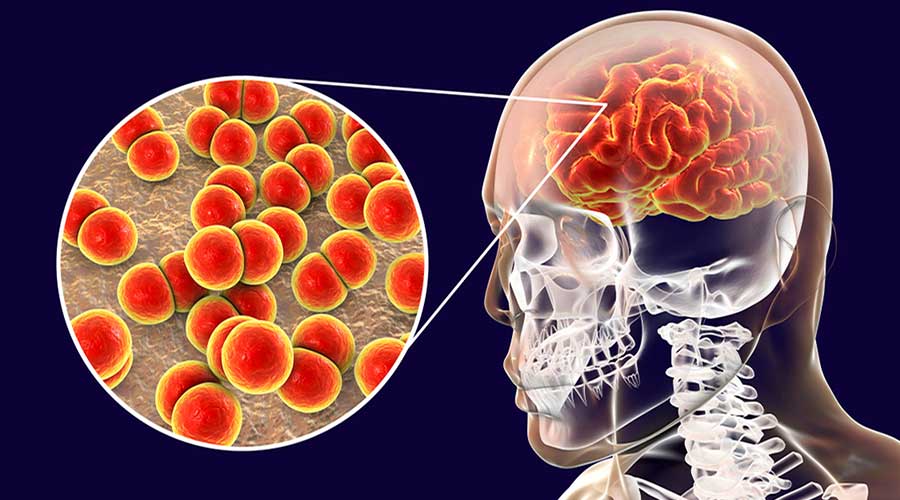
Neisseria meningitidis, commonly known as meningococcus, is a bacterium notorious for causing meningitis and other severe infections in humans. This pathogen poses a significant threat to public health worldwide, especially in densely populated settings like schools, military bases, and refugee camps. Meningococcal infections can lead to grave complications, including neurological damage and fatalities if left untreated.
The Concept of Bacterial Membranes and Porins
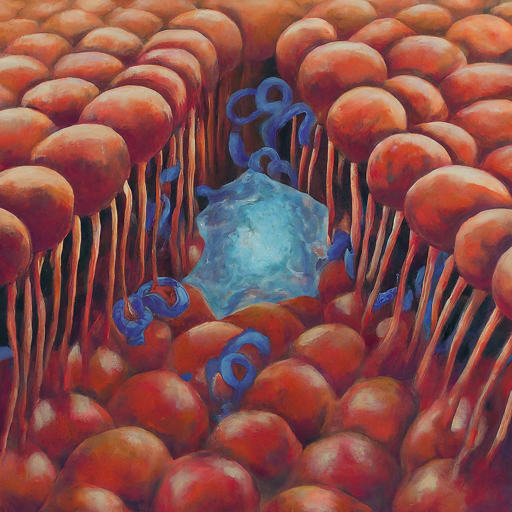
Bacterial membranes serve as critical barriers enveloping the cell, providing structural integrity and regulating the passage of molecules in and out of the cell. These membranes are composed of various components, including proteins like porins.
Porins are specialized proteins embedded within the bacterial outer membrane, forming channels that facilitate the diffusion of ions, nutrients, and other molecules across the membrane. They play a pivotal role in bacterial survival by facilitating the uptake of essential nutrients and the secretion of toxins.
Porins: Gateway Proteins for Bacterial Survival
Porins are specialized proteins embedded within the bacterial outer membrane, forming channels that facilitate the diffusion of ions, nutrients, and other molecules across the membrane. They play a pivotal role in bacterial survival by facilitating the uptake of essential nutrients and the secretion of toxins.
Focus on PorA: Functions, Immune Evasion, and Vaccine Target
PorA, a major outer membrane protein of Neisseria meningitidis, plays a crucial role as both a virulence factor and a prime target for the host immune system and vaccine development.
- PorA as a Porin:
- Aids in the passage of molecules across the bacterial outer membrane.
- Adhesion to Host Cells:
- Facilitates colonization and invasion by promoting the adhesion of meningococci to host cells.
- Immune Evasion through Antigenic Variation:
- Alters its surface structure through antigenic variation to evade antibody recognition, enabling meningococci to evade the host immune response.
Role in Immune Evasion:
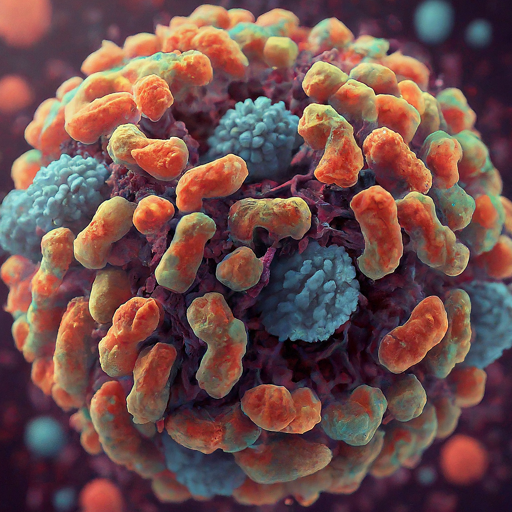
Meningococci employ antigenic variation of PorA through genetic recombination and phase variation to evade the host immune system. This mechanism enables the bacteria to escape antibody recognition, posing challenges for the immune system to mount an effective response.
Significance as a Vaccine Target:
- Given its pivotal role in meningococcal pathogenesis and immune evasion, PorA is a prime target for vaccine development.
- Vaccines targeting PorA aim to elicit protective immune responses against multiple strains of Neisseria meningitidis, thereby thwarting meningococcal disease.
- These vaccines typically incorporate PorA as a key antigen, either as part of outer membrane vesicle vaccines or as a recombinant protein in protein-based vaccines.
In conclusion, comprehending the role of PorA in Neisseria meningitidis pathogenesis and immune evasion is crucial for developing effective vaccines against meningococcal disease. PorA's functions as a porin, its involvement in immune evasion, and its significance as a vaccine target underscore its importance in combating this deadly pathogen and safeguarding public health.
Exploring PorA's Mechanisms : Insights into Bacterial Pathogenesis
Structural Characteristics of PorA:
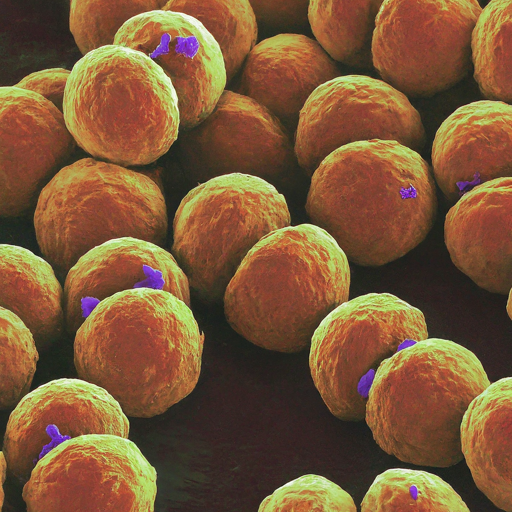
PorA exhibits a β-barrel structure, typical of outer membrane proteins in gram-negative bacteria. This structural arrangement enables PorA to form channels within the bacterial outer membrane, facilitating the passage of molecules essential for bacterial survival and virulence.
Interaction with Host Cells:
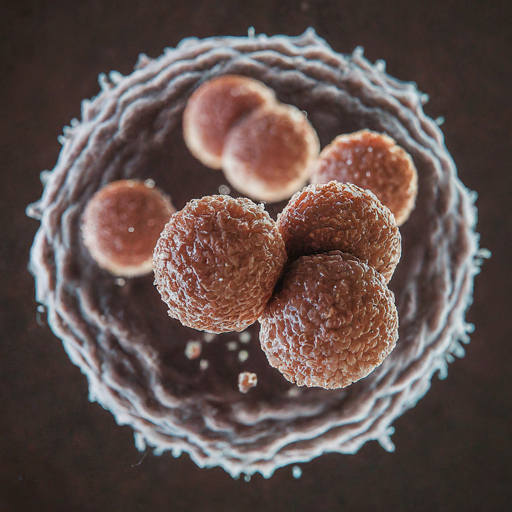
PorA interacts with various host cell receptors, facilitating the adhesion of Neisseria meningitidis to epithelial and endothelial cells. This interaction is crucial for the initial stages of infection, allowing the bacteria to establish colonization and evade host immune surveillance.
Modulation of Host Immune Response:
Apart from its role in antigenic variation, PorA influences the host immune response through various mechanisms. It can modulate the activation of immune cells, such as macrophages and dendritic cells, and interfere with the production of pro-inflammatory cytokines, thereby promoting bacterial survival within the host environment.
Impact on Disease Severity:
The expression levels and structural characteristics of PorA can influence the severity of meningococcal disease. Strains expressing certain PorA variants may exhibit enhanced virulence, leading to more severe clinical outcomes in infected individuals.
Targeting PorA for Therapeutic Interventions
Vaccine Strategies:
Efforts to develop vaccines targeting PorA have focused on eliciting protective immune responses against diverse strains of Neisseria meningitidis. Outer membrane vesicle vaccines containing PorA have been used successfully in some regions to control meningococcal outbreaks and reduce disease burden.
Challenges and Future Directions:
Despite advancements in vaccine development, challenges remain in achieving broad protection against the diverse array of meningococcal strains. Antigenic variation and the presence of non-PorA virulence factors necessitate the exploration of alternative vaccine strategies, such as multi-component vaccines targeting multiple bacterial antigens.
Therapeutic Potential:
In addition to vaccine development, PorA represents a potential target for novel therapeutic interventions against meningococcal infections. Strategies aimed at disrupting PorA-mediated adhesion or immune evasion mechanisms could complement existing treatment modalities and help combat antibiotic resistance.
Neisseria meningitidis: Unveiling the Secrets of PorA, a Key Player in Meningitis
Meningitis, a serious infection of the brain and spinal cord, can be caused by the bacterium Neisseria meningitidis, also known as meningococcus. This pathogen poses a significant threat, especially in crowded settings like schools and refugee camps. While vaccines exist, understanding the complexities of meningococcus, particularly its key protein PorA, is crucial for developing even more effective prevention strategies.

Imagine PorA as a tiny gateway on the meningococcus's outer shell. This protein acts like a selective doorman, allowing essential nutrients in while keeping harmful substances out. But it's not just a passive gatekeeper. PorA also helps meningococcus stick to human cells, initiating infection, and can even change its disguise (antigenic variation) to evade the immune system.
This dual role of PorA makes it a double-edged sword:
- Virulence factor: PorA helps meningococcus survive and cause disease.
- Vaccine target: By targeting PorA, we can train the immune system to recognize and attack the bacteria.
Current vaccines often contain PorA, either as part of the bacterial outer membrane or as a purified protein. These vaccines have saved countless lives, but new strains with different PorA variations emerge, posing challenges.
Scientists are unlocking more secrets about PorA:
- Structure: Understanding how PorA is built helps us design drugs that block its function.
- Host cell interaction: Knowing how PorA interacts with human cells helps us develop therapies to prevent infection at its earliest stages.
- Disease severity: Different PorA variations might influence the severity of illness, helping us predict outcomes and personalize treatment.
The future of fighting meningococcal disease lies in:
- Next-generation vaccines: Vaccines targeting multiple meningococcal proteins, not just PorA, are under development.
- Novel therapies: Disrupting PorA's functions or its ability to evade the immune system could offer new treatment options.
By understanding PorA, we can unlock the secrets to defeating meningococcus and protecting communities from this dangerous disease.
Unraveling PorA's Structural Features
Beta-Barrel Architecture:
PorA adopts a characteristic β-barrel structure, typical of outer membrane proteins in gram-negative bacteria. This structural arrangement enables PorA to span the bacterial outer membrane, forming channels that facilitate the passage of ions, nutrients, and other molecules essential for bacterial survival and virulence.
Dynamic Surface Loops:
PorA exhibits surface-exposed loops that undergo dynamic conformational changes, contributing to its antigenic variability. These loops play a crucial role in immune evasion by altering the surface epitopes recognized by host antibodies, thereby confounding the host immune response and promoting bacterial persistence.
PorA-mediated Adhesion and Colonization
Host Cell Receptor Interactions:
PorA interacts with specific receptors on the surface of host cells, facilitating the adhesion of Neisseria meningitidis to epithelial and endothelial cells. This initial step is critical for establishing bacterial colonization within the host nasopharynx and initiating the cascade of events leading to invasive disease.
Biofilm Formation:
PorA contributes to the formation of bacterial biofilms, intricate communities of bacteria encased within a self-produced extracellular matrix. Biofilm formation enhances bacterial survival and persistence within the host environment, providing a sanctuary against host immune defenses and antimicrobial agents.
PorA and Host Immune Modulation
Immune Cell Activation:
PorA modulates the activation of immune cells, including macrophages, dendritic cells, and T cells, through various signaling pathways. By influencing the production of pro-inflammatory cytokines and chemokines, PorA can shape the host immune response to promote bacterial survival and dissemination.
Evasion of Complement-mediated Killing:
PorA contributes to the evasion of complement-mediated killing, a key component of the innate immune response against bacterial pathogens. By interfering with the activation of the complement cascade or binding complement regulatory proteins, PorA enables Neisseria meningitidis to evade destruction by the host complement system.
PorA as a Therapeutic Target
Vaccine Development:
PorA represents a prime target for vaccine development against meningococcal disease. Vaccines incorporating PorA as a key antigen aim to elicit protective immune responses, including antibody-mediated clearance and cell-mediated immunity, against diverse strains of Neisseria meningitidis.
Novel Therapeutic Approaches:
Beyond traditional vaccine strategies, innovative therapeutic approaches targeting PorA are under investigation. These include monoclonal antibody therapies, small molecule inhibitors of PorA-mediated adhesion, and immunomodulatory agents aimed at enhancing host immune responses against Neisseria meningitidis.
Conclusion
PorA, as a key component of Neisseria meningitidis, plays multifaceted roles in bacterial pathogenesis, immune evasion, and vaccine development. Understanding the intricate mechanisms underlying PorA function is essential for devising effective strategies to combat meningococcal disease and safeguard public health.
PorA stands at the forefront of Neisseria meningitidis pathogenesis, playing multifaceted roles in bacterial adhesion, immune evasion, and vaccine development. Understanding the intricate mechanisms underlying PorA function holds immense promise for the development of novel therapeutic interventions and the effective control of meningococcal disease.
- How does PorA contribute to bacterial survival?
- PorA facilitates the uptake of essential nutrients and the secretion of toxins, aiding in bacterial survival within the host environment.
- What challenges does antigenic variation of PorA pose for vaccine development?
- Antigenic variation of PorA allows meningococci to evade antibody recognition, making it challenging to develop vaccines that effectively target this protein and provide broad protection against diverse strains.
- Are there any specific vaccine formulations targeting PorA?
- Yes, some vaccines incorporate PorA as a key antigen to induce protective immune responses against Neisseria meningitidis. These formulations may include PorA in outer membrane vesicle vaccines or as a recombinant protein in protein-based vaccines.
- How does PorA contribute to the adhesion of meningococci to host cells?
- PorA promotes the adhesion of meningococci to host cells by interacting with specific receptors on the surface of epithelial and endothelial cells. This interaction facilitates bacterial colonization and invasion, initiating the onset of meningococcal disease.
- What are the potential consequences of untreated meningococcal infections?
- Untreated meningococcal infections can lead to severe complications, including neurological damage, septicemia, and fatalities. Prompt diagnosis and appropriate medical intervention are essential to prevent adverse outcomes associated with meningococcal disease.
- How does PorA influence the pathogenicity of Neisseria meningitidis?
- PorA contributes to the pathogenicity of Neisseria meningitidis by facilitating bacterial adhesion, colonization, and evasion of the host immune response. Its role as a porin and in antigenic variation enhances the bacterium's ability to survive and cause disease.
- Can PorA be targeted for novel antimicrobial therapies?
- Yes, PorA represents a potential target for novel antimicrobial therapies aimed at disrupting bacterial adhesion, colonization, or immune evasion mechanisms. Strategies such as small molecule inhibitors or monoclonal antibodies targeting PorA may offer alternative approaches to combat meningococcal infections.
- What factors influence the expression levels of PorA in Neisseria meningitidis?
- The expression levels of PorA in Neisseria meningitidis can be influenced by various factors, including environmental conditions, host factors, and regulatory mechanisms within the bacterium. Changes in expression may impact bacterial virulence and pathogenicity.
- Are there any known interactions between PorA and other bacterial proteins or host factors?
- Yes, PorA may interact with other bacterial proteins or host factors to modulate bacterial pathogenesis and immune responses. Further research is needed to elucidate these interactions and their implications for meningococcal disease.
- How does PorA contribute to the development of meningococcal resistance to antibiotics?
- While PorA itself does not directly contribute to the development of antibiotic resistance in Neisseria meningitidis, its role in bacterial survival and pathogenicity may indirectly influence the emergence of resistance mechanisms. Understanding PorA's involvement in bacterial physiology can inform strategies to mitigate antibiotic resistance.